What Is COBRA Insurance and How Much Does It Cost?
COBRA allows you to temporarily keep the health insurance from your job even after you leave your employer.
Find Cheap Health Insurance Quotes in Your Area
But COBRA tends to be expensive because your job no longer helps you pay for the monthly cost of coverage. Instead, you have to pay the full rate. Nationally, COBRA costs an average of $750 per month for one person or $2,196 per month for a family. Buying a plan from HealthCare.gov or your state's marketplace is often a cheaper option.
What is COBRA insurance?
COBRA insurance gives you the option to hold on to your employer health plan after you stop working.
This means you can keep seeing your primary care doctor and any specialists, and all the same services will be covered. COBRA helps you avoid gaps in your coverage, but you'll pay more because your company will no longer pay part of the bill.
What does COBRA stand for?
COBRA stands for the Consolidated Omnibus Budget Reconciliation Act. This is a law that lets you and your family keep the health insurance from your job even if you quit, are fired (for most reasons) or retire. You can also keep your coverage through COBRA if your hours are cut so much that you don't qualify for your employer's health insurance anymore.
COBRA usually only applies to companies that have 20 or more employees, so if you work for a very small business, you might not have access to COBRA coverage.
How much is COBRA insurance?
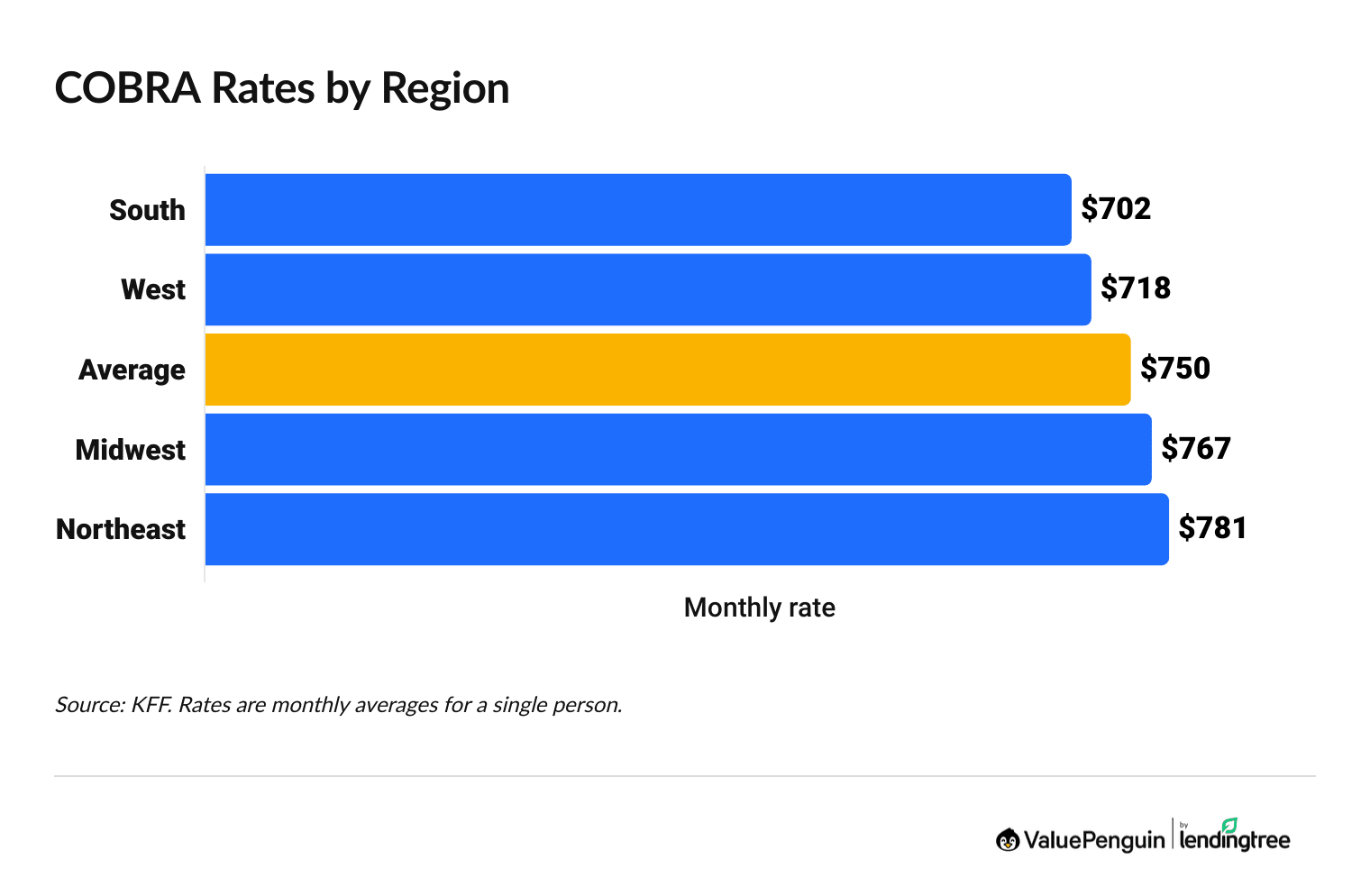
On average, COBRA costs $750 for a single person and $2,196 per month for a family.
Costs depend on where you live, among other things. COBRA tends to be a bit cheaper in the South and West, although the Midwest isn't much more expensive. People who live in the northeastern part of the United States typically pay the highest rates for COBRA coverage.
Find Cheap Health Insurance Quotes in Your Area
Your employer won't pay any of the cost for your plan once you're on COBRA. On average, when you have a job, employers pay about 84% of the cost for a single person's health insurance and about 74% of the cost for a family plan.
But when you leave your job and get on COBRA, you have to pay the entire monthly rate. This means you'll pay between about 4 and 6 and a quarter times more for health insurance compared to when you were still at your job.
COBRA rates by state
State | Region | Indv. rate | Family rate |
|---|---|---|---|
| Alabama | South | $702 | $2,087 |
| Alaska | West | $718 | $2,159 |
| Arizona | West | $718 | $2,159 |
| Arkansas | South | $702 | $2,087 |
| California | West | $718 | $2,159 |
Source: KFF. Rates are for the Northeast, Midwest, South and West regions and are not state specific.
You may also pay an extra 2% charge for plan administration. This is an optional fee that some insurance companies charge to cover the cost of things like paperwork, customer service and claim review.
What affects COBRA costs?
- Your employer contributions: The more your employer paid toward your health insurance, the more your monthly payments will increase once COBRA starts, because you'll be taking on the full cost of your health plan.
- Pretax versus after-tax income: Health insurance payments from your paycheck are usually made with pretax dollars. However, your COBRA rates will likely be paid with your after-tax income. That means your tax bill might go up at the end of the year.
- HMO or PPO: Health maintenance organizations (HMOs) tend to be cheaper than preferred provider organizations (PPOs). That's because HMOs restrict you to a network of doctors, while PPOs let you go to any doctor and still have some coverage.
- Plan choices: The plan options made available by your employer will influence your final cost, because some health plans have better coverage and higher rates.
- Insurance company: Some companies charge lower rates than others.
How does COBRA insurance work?
COBRA works by letting you stay on your employer's health coverage for up to 18 months after you've lost your job.
Spouses and dependent children can stay on COBRA for 36 months in some cases, such as divorce or death.
After you lose your job, your employer has two weeks to tell you about your COBRA options. Then, a 60-day window opens, during which you can accept or decline COBRA coverage. You can sign up for COBRA at any time during that period, even if you initially declined. Keep in mind that every person in your household has to individually sign up for COBRA. So if your health insurance covers you, a spouse and a child, all three of you need to select that you want COBRA coverage. Parents and guardians can select COBRA for children.
You can also sign up for an individual health plan during the first two months after you lose your job. You can do that because of what's called a "special enrollment period." This lets you get health insurance outside of the normal time frame in the fall, called open enrollment.
How to get COBRA insurance
After you lose your job, your former employer will notify you by mail or email about your rights under COBRA. This communication will include eligibility requirements and COBRA application instructions.
You may have to submit documents proving your eligibility. For example, if you're separating from your spouse, you might be asked for a certified copy of your divorce decree to qualify for the extended 36-month COBRA coverage period.
COBRA eligibility requirements
- You must be enrolled in your group health plan before losing your job. In addition, you must have had that insurance for more than half the days you worked in the previous year.
- You were laid off, you were fired for any reason except gross misconduct or you lost your health insurance because your hours were reduced. Gross misconduct refers to serious firing offenses, such as theft, workplace violence and sexual harassment. If you're fired for gross misconduct, you won't be eligible for COBRA.
- Your workplace has at least 20 full-time employees. You can add hours for part-time employees to get a full-time employee equivalent. For example, two employees who each work 20 hours a week would be considered one full-time employee.
- You work for a business or a local or state government. Federal employees are not eligible for COBRA, although they have access to a similar program. COBRA doesn't apply to churches or some religious groups.
- Your organization must continue to offer health insurance after you leave. If your employer goes out of business or stops offering health insurance to existing employees, you may lose your COBRA eligibility.
Some states require small businesses to offer COBRA-like coverage even if they don't meet the 20 full-time employee threshold. The rules governing these programs, also known as mini-COBRA, vary from state to state, so it's important to check your local rules if you think you might be eligible.
Spouses and dependent children can get COBRA under all of the above circumstances. Both groups can also get COBRA in a few other situations.
If you get your health insurance through your spouse and they lose their job, you can get COBRA if:
- You divorce or become legally separated.
- Your spouse enrolls in Medicare.
- Your spouse dies.
Children who get health insurance through a parent or guardian who loses their job can get COBRA if:
- The parent enrolls in Medicare.
- They no longer qualify as a dependent child.
COBRA insurance deadlines
COBRA is only available for a short period of time after you lose your job. It's important to enroll in COBRA within 60 days to prevent a lapse in health coverage.
Deadline | Action |
|---|---|
| 14 days | Your employer must contact you about your COBRA eligibility |
| 60 days | You must enroll or decline COBRA |
Alternatives to COBRA
COBRA isn't the only way to avoid a lapse in health insurance coverage if you lose your job.
You can also consider buying an "Obamacare" plan on HealthCare.gov or your state's marketplace site or getting a short-term plan.
"Obamacare" plans are plans you buy from HealthCare.gov or your state's health insurance marketplace site. These plans have good coverage, are often cheaper than COBRA and you can buy one within 60 days of losing your job.
Marketplace plans come in different levels: Catastrophic, Bronze, Silver, Gold and Platinum. The more health care you need, the higher plan tier you should buy.
Plan tier | Monthly rate |
|---|---|
| Catastrophic | $434 |
| Bronze | $573 |
| Silver | $752 |
| Gold | $793 |
| Platinum | $1,012 |
Average rate for a 40-year-old.
If you're young and in good health, you could consider a Catastrophic health insurance plan. Catastrophic plans are cheap, which can be appealing if you're out of work. But you have to pay the first $10,600 of your medical bills yourself, so it's important to have savings in the bank.
If you are willing to pay a bit more, a Bronze or Silver plan is a better option. You'll pay a higher monthly rate, but less when you go to the doctor. And if you have frequent or expensive medical needs, go with a Gold or Platinum plan.
Before you sign up for COBRA, check to see if you qualify for Affordable Care Act (ACA) subsidies, also called premium tax credits. These discounts can make private health insurance a more affordable option than COBRA, but you can't use them on Catastrophic plans.
Short-term health insurance can be a good option if you only need coverage for a few weeks or months between jobs. However, these policies usually don't have coverage as good as group or HealthCare.gov plans.
For example, all regular health insurance plans must cover mental health because it's considered an essential benefit under the ACA. However, a short-term health policy might not offer mental health coverage. You could also be denied for having preexisting conditions. That can't happen with a plan you get from the marketplace.
Frequently asked questions
What is COBRA insurance and how does it work?
COBRA is a law that lets you continue the health insurance you had from your job even after you quit, retire or are fired (for most reasons). Usually, COBRA lets you keep your plan for a year and a half after you lose your job, but the coverage can last up to three years in some cases.
How much does COBRA cost per month?
For one person, COBRA costs $750 per month, on average. For a family, the average is $2,196 per month. Rates depend on where you live, the company that provides your coverage and the specific plan and coverage you chose from your job.
What are the disadvantages of COBRA insurance?
The main drawback of COBRA coverage is that it can be expensive. When you're working, your employer pays for a large share of your health insurance rate. Most employers pay about 84% of the total cost for a plan, which means you only pay 16%. But when you get on COBRA, you have to pay the full cost for a plan. You can often get a cheaper plan through HealthCare.gov or a state marketplace site, especially if you can get monthly discounts called subsidies.
Sources and methodology
Average group health insurance rates are from KFF. COBRA rules and regulations are from the U.S. Department of Labor.
Monthly rates for marketplace places are from the Centers for Medicare & Medicaid Services (CMS) public use files and are for 2026. Rates are for a 40-year-old. Not every plan tier is available in every state.
About the Author
Insurance Writer
Cate Deventer is a ValuePenguin writer who specializes in health insurance, Medicare, auto and home insurance. She's been a licensed insurance agent since 2011.
She started her insurance career working as a customer service agent for State Farm. She later moved to an independent agency, where she worked with several insurance companies and hundreds of clients. She quoted policies, filed claims and answered insurance questions. In 2021, she pivoted her career and began writing about insurance for Bankrate. She moved to ValuePenguin in 2023 and began writing about health insurance and Medicare.
Cate has a passion for helping readers choose insurance to fit their needs. She enjoys knowing that her research and knowledge help people choose insurance products that make a positive difference in their lives.
How insurance helped Cate
Cate used her health insurance knowledge to navigate a surgery in 2023. Understanding how her policy worked let her focus on recovery instead of worrying about bills.
Expertise
- Health insurance
- Medicare & Medicaid
- Auto insurance
- Home insurance
- Life insurance
Credentials
- Licensed Life, Accident & Health Insurance Agent
- Licensed Property & Casualty Insurance Agent
Referenced by
- CBS
- NBC
- Wall Street Journal
Education
- BA, Theatre, Purdue University
- BA, English, Indiana University
Editorial note: The content of this article is based on the author's opinions and recommendations alone. It has not been previewed, commissioned or otherwise endorsed by any of our network partners.
