Largest Health Insurance Companies
The five largest health insurance companies are UnitedHealth Group, Kaiser Permanente, Anthem, Ambetter and HCSC (Blue Cross Blue Shield).
Find Cheap Health Insurance Quotes in Your Area
5 largest health insurance companies
What are the biggest health insurance companies?
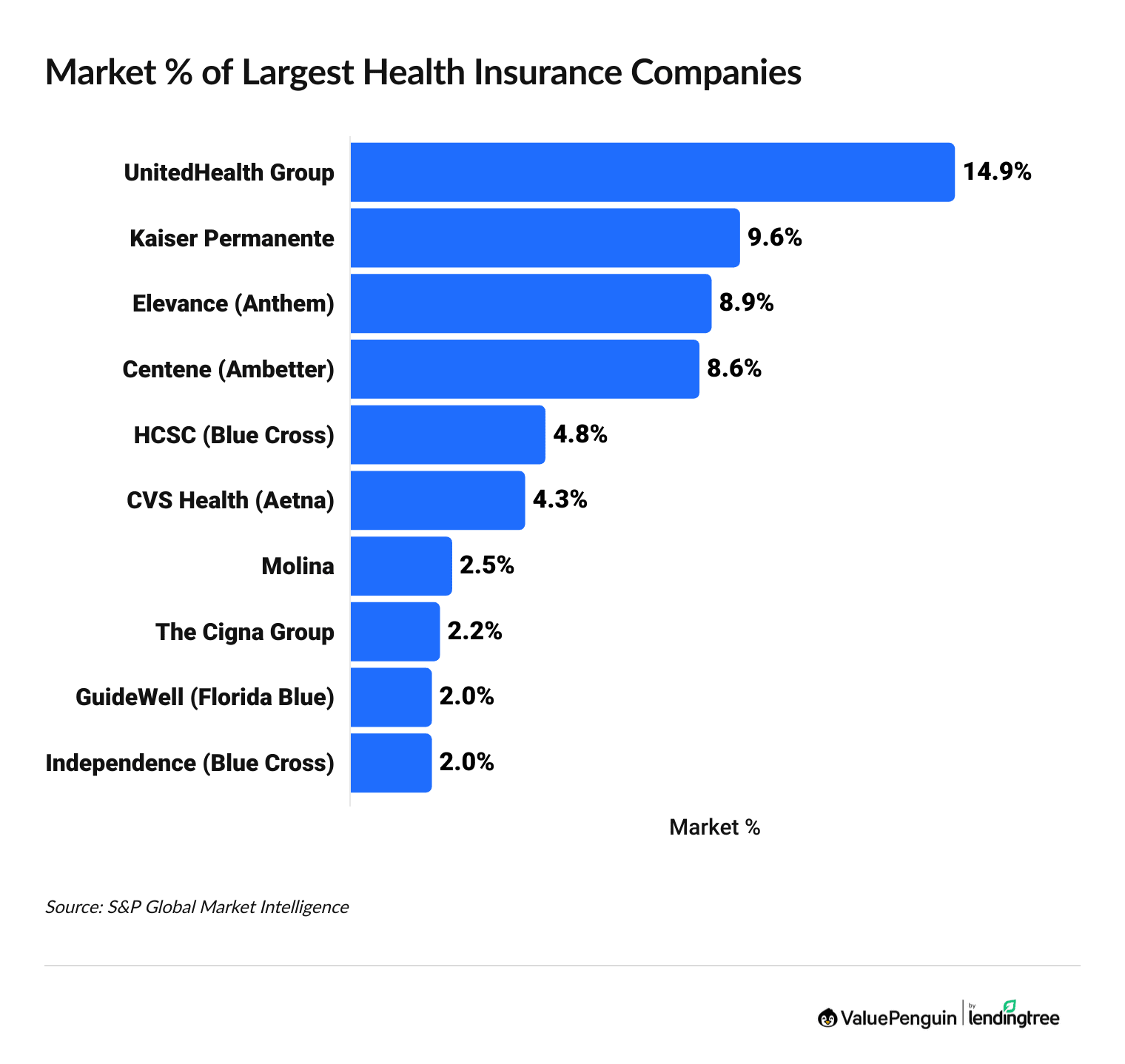
UnitedHealth Group, Kaiser Permanente, Elevance (Anthem), Centene (Ambetter) and HCSC (Blue Cross Blue Shield) are the five biggest health insurance companies and make up nearly half of the health insurance market.
Find Cheap Health Insurance in Your Area
List of largest health insurance companies by revenue
Company | Market share | Revenue (billions) | |
|---|---|---|---|
| UnitedHealth Group | 14.9% | $224B | |
| Kaiser Permanente | 9.6% | $144B | |
| Elevance Health (Anthem) | 8.9% | $134B | |
| Centene (Ambetter) | 8.6% | $130B | |
| HCSC (Blue Cross) | 4.8% | $73B |
Revenue is rounded to the nearest billion.
Top 5 largest health insurance companies
Each of the largest health insurance companies has millions of customers. You can enroll in a health insurance policy from one of the largest companies in many different ways.
For example, your employer's benefit plan may offer health insurance, or you can buy a private insurance plan through the Affordable Care Act (ACA) marketplace, also called "Obamacare."
1. UnitedHealth Group
-
Editor rating
- Revenue: $224B
- Market share: 14.9%
- Enrollment: 5,686,907
UnitedHealthcare, part of UnitedHealth Group, is the largest health insurance company, based on revenue. UnitedHealthcare sells individual and family plans, as well as group plans, which you get through an employer.
UnitedHealthcare also has a network of over 1.3 million doctors and health care professionals, with more than 6,500 hospitals. This means that if you have UnitedHealthcare, you will have many options for where you can get medical care.
You can buy policies individual and family plans from UnitedHealthcare in 30 states. UnitedHealthcare is headquartered in Minnetonka, MN.
2. Kaiser Permanente
-
Editor rating
- Revenue: $144B
- Market share: 9.6%
- Enrollment: 8,549,366
Kaiser Permanente is the second-largest provider of health insurance in the U.S. by revenue but the largest by enrollment for group and individual health insurance. Much of its membership comes from group health insurance plans from employers. The company also sells low-cost plans across a variety of coverage types, including individual health insurance, Medicare Advantage and Medicaid.
Kaiser Permanente only sells policies in eight states and Washington, D.C., but it's very popular where it's available. The insurance company's focus is on low-cost HMO plans that require you to use one of Kaiser's medical centers to get health care, unless it's an emergency.
3. Elevance (Anthem)
-
Editor rating
- Revenue: $134B
- Market share: 8.9%
- Enrollment: 6,297,307
Anthem, which is part of Elevance Health, is the third-largest medical insurance provider by revenue and has nearly 6.3 million health insurance members. The company offers insurance to large and small businesses, individuals and families.
The company currently only sells plans in 14 states.
Anthem is part of the Blue Cross Blue Shield Association, which, in total, covers all 50 states. This can give you some benefits like nationwide access to medical care through the BlueCard program, which lets you use your coverage easily when you're traveling. The Blue Cross Blue Shield provider network is the largest in the country and includes about 90% of doctors and hospitals.
4. Centene (Ambetter)
-
Editor rating
- Revenue: $130B
- Market share: 8.6%
- Enrollment: 5,690,745
Centene is a large health insurance company, and most of its health insurance plans come from Ambetter. As a company, Centene is the fourth-largest major medical insurance company in the United States by revenue. It sells the most individual health insurance plans of any company, with 4,480,374 members in 2024.
Ambetter is one of Centene's main individual health insurance companies. But Ambetter doesn't sell Medicare Advantage or Medicare Part D plans. Instead, Wellcare is the main Centene subsidiary selling these policies.
Centene was started in 1984 as a provider of Medicaid plans, and today, it's the largest provider of managed care Medicaid plans — where a health insurance company oversees Medicaid benefits — in the country.
5. HCSC (Blue Cross Blue Shield)
-
Editor rating
- Revenue: $73B
- Market share: 4.8%
- Enrollment: 5,560,234
HCSC, which stands for Health Care Service Corporation, is the fifth-largest health insurance company by revenue and enrollment, with nearly 5.6 million customers. The company's name may not be familiar to most people, but HCSC operates Blue Cross Blue Shield companies in Illinois, Montana, Nevada, Oklahoma and Texas.
In addition to managing health insurance companies, HCSC also works with local nonprofits in the communities it serves. HCSC provides funding to nonprofits that help improve nutrition, economic development, housing and more.
HCSC was founded in 1936. Today, the company also owns brands such as Collective Health, the Dearborn Group and Prime Therapeutics.
HCSC is just one of many Blue Cross Blue Shield companies. If you were to put all the subsidiaries together, BCBS would be the largest health insurance company in the country.
Major health insurance companies by state
Blue Cross Blue Shield is the largest health insurance company by membership in most states. That includes affiliates like Elevance (Anthem), Highmark and CareFirst.
State | Company |
|---|---|
| Alabama | Blue Cross Blue Shield of Alabama |
| Alaska | Premera Blue Cross |
| Arizona | Prosano (Blue Cross Blue Shield) |
| Arkansas | Arkansas BlueCross BlueShield |
| California | Kaiser Permanente |
Largest company by enrollment for both individual and group insurance.
Largest health insurance companies by enrollment
Kaiser Permanente is the largest health insurance company in the country by enrollment.
The company has over 8.5 million members with either an individual or group health insurance plan. Even though Kaiser's plans are only sold in eight states and Washington, D.C., it has high enrollment in the states where it is available.
But Kaiser Permanente doesn't have the highest revenue because it sells cheap health insurance plans. Anthem has the second-largest membership, followed by Centene (Ambetter).
10 biggest health insurance companies by enrollment
Company | 2024 enrollment | |
|---|---|---|
| Kaiser Permanente | 8.5 million | |
| Elevance Health (Anthem) | 6.3 million | |
| Centene (Ambetter) | 5.7 million | |
| UnitedHealth Group | 5.7 million | |
| HCSC (Blue Cross) | 5.6 million |
Individual and employer health insurance plans
Blue Cross Blue Shield (BCBS) is a big health insurance company, but it's actually a collection of different individual companies. Of the 10 health insurance companies with the most members, five are part of BCBS. If all BCBS companies were combined, they would have the largest health insurance enrollment in the U.S.
Frequently asked questions
What are the five largest health insurance companies?
The five largest health insurance companies by revenue are UnitedHealth Group, Kaiser Permanente, Anthem, Centene (mostly Ambetter) and HCSC (part of Blue Cross Blue Shield). They make up about half of the total market share in the health insurance industry. UnitedHealthcare has the highest revenue, earning nearly $224 billion in 2024. But Kaiser Permanente has the highest enrollment. Over 8.5 million people have Kaiser Permanente plans.
Who is the #1 provider of health insurance in the U.S.?
Kaiser Permanente has the most health insurance plans of any company in the U.S., with more than 8.5 million members. About 7.5 million Kaiser Permanente members have group health insurance plans that are sold through an employer. Another million people have an individual Kaiser Permanente plan that they purchased on HealthCare.gov or a state marketplace. You can only get Kaiser Permanente in eight states, but it's one of the best health insurance companies where it's available.
Should you choose a large health insurance company when buying a plan?
Getting coverage from a big company can be helpful. The biggest health insurance companies usually have a large network of doctors and medical providers, which gives you options for where you get your medical care. But poor customer service is a common complaint about big insurance companies, and there are several smaller companies that have better customer satisfaction.
Methodology
Data on market share, revenue and enrollment is from S&P Capital IQ, pulled in August 2025, and based on the most recent annual data available — for the calendar year of 2024. Enrollment data includes group and individual health insurance plans, but not Medicare or Medicaid. National enrollment and California enrollment are reported separately but have been combined.
Editorial note: The content of this article is based on the author's opinions and recommendations alone. It has not been previewed, commissioned or otherwise endorsed by any of our network partners.















