Best Cheap Health Insurance in New York for 2026
MVP Health Care offers the best health insurance in New York. Bronze plans start at $671 per month before discounts.
Find Cheap Health Insurance Quotes in New York
Best and cheapest health insurance in New York
Cheapest health insurance companies in New York
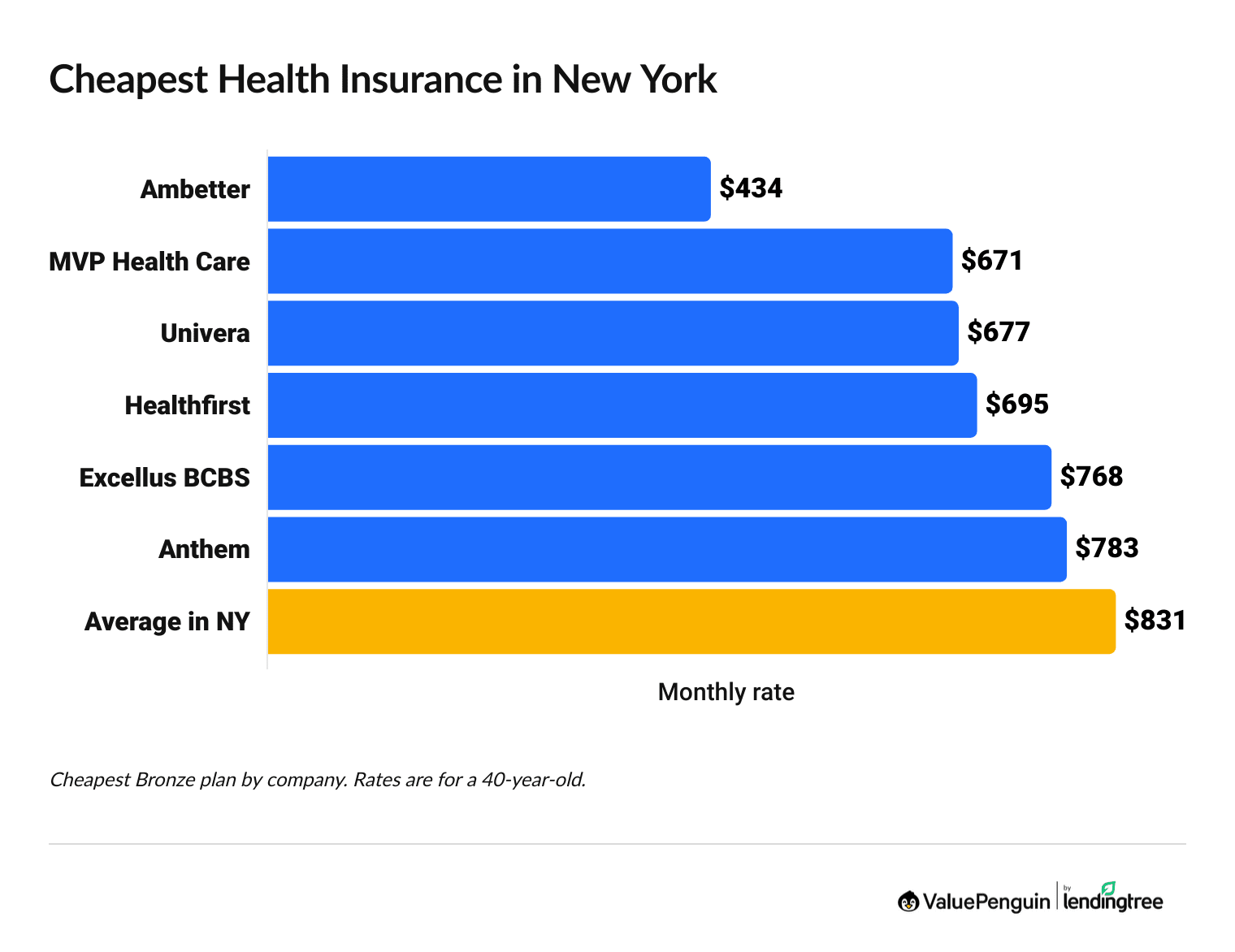
Ambetter from Fidelis Care, MVP Health Care and Univera have the cheapest health insurance plans in New York, with Bronze plans starting at $434 per month before discounts.
Find Cheap Health Insurance Quotes in New York
Affordable health plans in NY
Company |
Cost
| |
|---|---|---|
| Ambetter from Fidelis Care | $434-$702 | |
| MVP Health Care | $671-$982 | |
| Univera | $677-$765 | |
| Healthfirst | $695-$807 | |
- Ambetter from Fidelis Care's cheapest Bronze plan costs $434 each month. That's just over half the average for a Bronze plan in New York State.
- Ambetter from Fidelis Care also sells the most affordable Bronze medical insurance in all five boroughs of New York City. But the best coverage in NYC comes from Anthem.
Best health insurance companies in New York
MVP Health Care has the best health insurance for most New Yorkers.
MVP has a high 4-star rating from NY State of Health, the New York health insurance marketplace. And MVP gets a perfect 5-star rating for member experience, which means it has excellent customer service.
Find Cheap Health Insurance Quotes in New York
Best-rated health insurance companies in New York
Company |
ACA rating
|
VP rating
|
|---|---|---|
| MVP Health Care | ||
| Independent Health | N/A | |
| MetroPlus Health Plan | ||
| UnitedHealthcare | ||
| Excellus BCBS |
If you live in western New York, Independent Health is the best insurance company.
Independent Health only sells plans in eight counties in the western part of New York, so it's not an option for most people in the state.
Independent Health has a reputation for excellent customer service, with 91% fewer complaints compared to an average company its size. Bronze plans from Independent Health start at $786 per month.
Best health insurance in NYC: Anthem
Anthem is the best health insurance company for people living in New York City, with Bronze plans starting at $822 per month in NYC per month before discounts.
Not only does the company sell plans in the five boroughs of NYC, but it gives you access to a wide range of doctors and hospitals. Anthem is part of Blue Cross Blue Shield, which has one of the largest doctor networks in the country.
However, Anthem isn't the cheapest option in NYC. Ambetter from Fidelis Care sells the cheapest medical insurance in New York City, with rates starting at $675 per month for a Bronze plan — but its plans will usually have higher deductibles compared to plans from Anthem. Choosing a plan with a lower deductible means your coverage starts sooner.
How much does health insurance cost in New York?
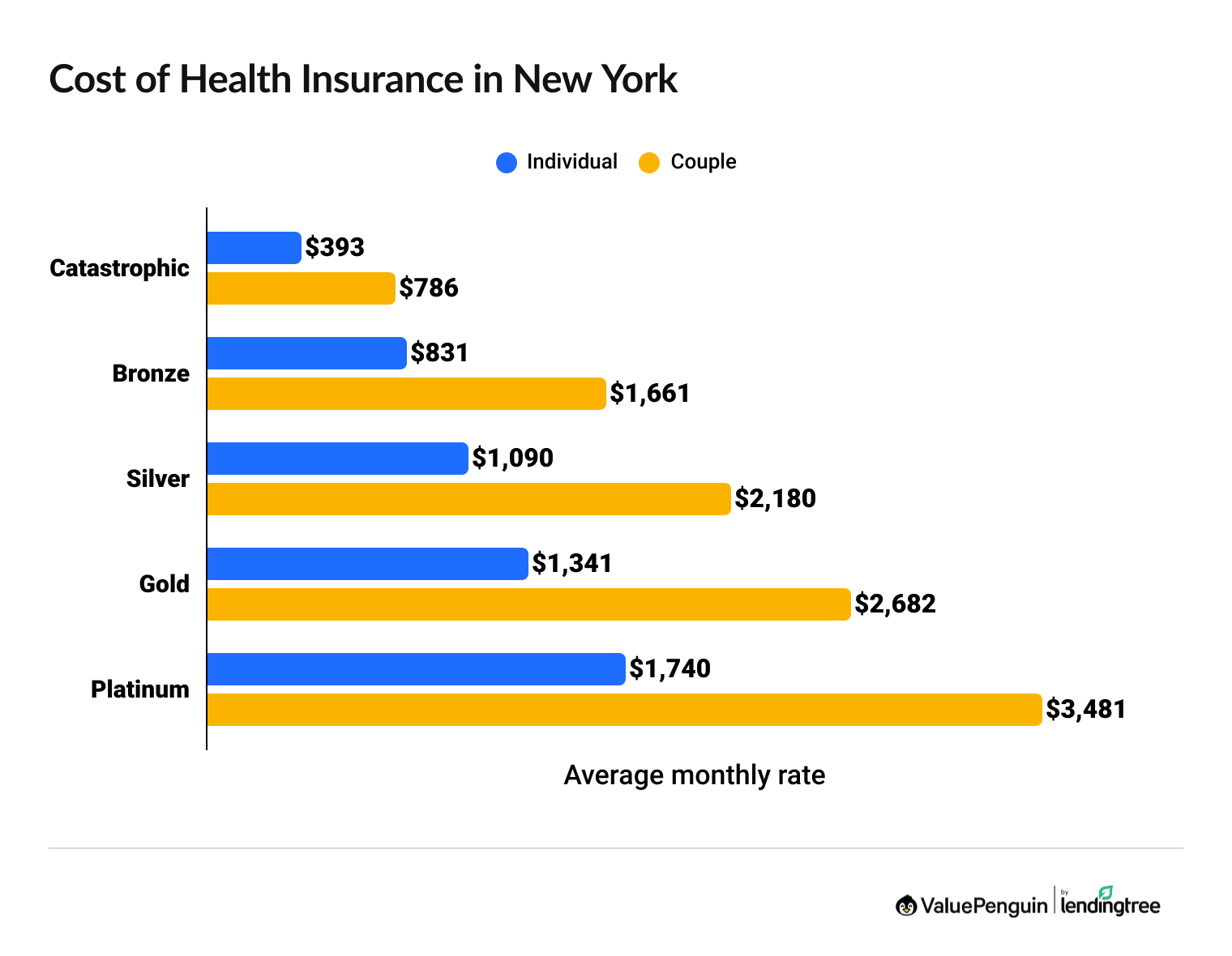
Health insurance in New York costs an average of $1,090 per month for a Silver plan and $831 per month for a Bronze plan, but you could pay an estimated $534 per month after discounts.
Find Cheap Health Insurance Quotes in New York
- Platinum and Gold plans have expensive monthly rates, but you pay less when you visit the doctor or get a prescription filled. Bronze plans have cheap monthly rates and high costs when you get medical care.
- Silver health plans have middle-of-the-road rates and costs when you see the doctor. However, Silver plans are only a good option in New York if you make more than $39,125 per year. If you make less than that, you can get the New York Essential Plan, a free health plan for people with low incomes.
In New York, your health insurance rate won't change because you get older.
Your rate also won't change if you smoke or use other tobacco products.
Health insurance discount changes in New York for 2026
Health insurance is estimated to cost about $534 per month in New York if you can get discounted rates because of your income.
If you got discounts in 2025, you can expect your rates to go up by about $200 in 2026. In 2025, the average cost of health insurance in New York after subsidies was $336 per month. In 2026, the cost is expected to be about $534 per month.
The increase is because of a likely change to the size of the discounts. Since 2021, discounts on the marketplace have been bigger. These "enhanced subsidies" are expiring at the end of 2025. People with the lowest incomes will see the biggest changes in their rates.
Health insurance rates in New York after subsidies (2025 vs. 2026)
Income | 2025 rate | 2026 rate | Difference |
|---|---|---|---|
| $40,000 | $154 | $287 | 86% |
| $50,000 | $283 | $415 | 47% |
| $60,000 | $423 | $498 | 18% |
| $70,000 | $496 | $817 | 65% |
| $80,000 | $567 | $817 | 44% |
Average cost after subsidies for a single 40-year-old with a Benchmark Silver plan.
If you make $39,125 or less, you can get the New York Essential Plan for free.
- What are subsidies? Subsidies are discounts that lower the cost of your monthly health insurance rate.
- How do you get subsidies? To get a subsidy, you have to make between $15,650 and $62,600 per year as an individual or between $32,150 and $128,600 per year as a family of four. NY State of Health will automatically check your eligibility for subsidies when you fill out your income on the website. However, laws around subsidies are rapidly changing and these numbers could be different very soon. You’ll also have to shop on NY State of Health — if you buy a plan directly from an insurance company, you won't be eligible for discounts.
- How much do subsidies save you? On average, subsidies save you $563 per month off the cost of a Silver plan. You can use ValuePenguin's subsidy calculator to see how much you could save.
- What plans can you use subsidies on? You can use subsidies to get cheaper rates on any Bronze, Silver, Gold or Platinum plan. You can't use subsidies on Catastrophic plans.
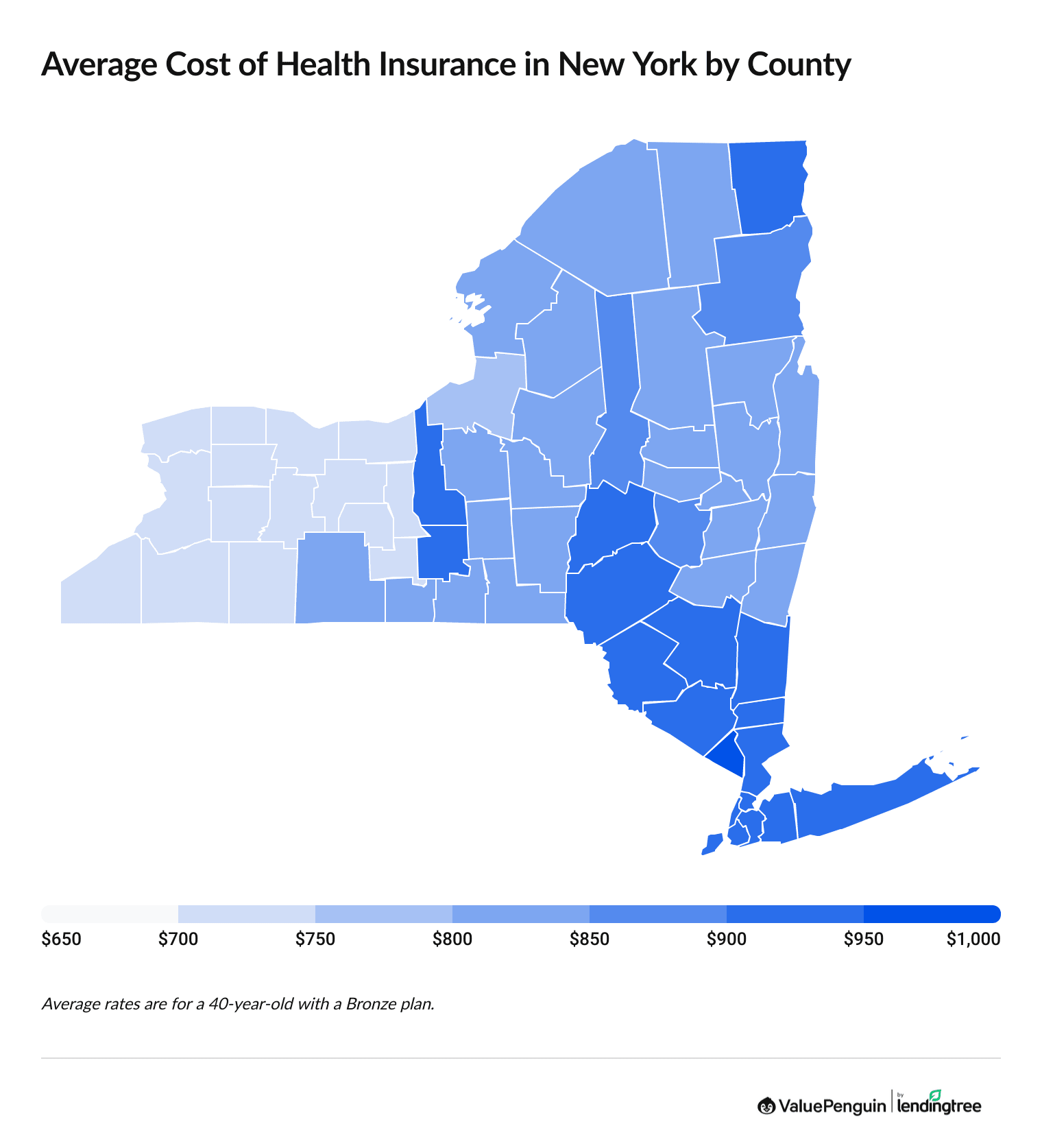
Average cost of health insurance by NY county
Health insurance rates in New York range between $706 and $951, on average, for a Bronze plan, depending on the county where you live.
Counties in western New York have the cheapest rates, while the southeast part of the state, near New York City and Long Island, pay the highest rates. Residents in Rockland County pay the highest rates, with a Bronze plan costing $951 per month, on average.
Average Bronze health insurance rates by NY county
NY county | Monthly rate |
|---|---|
| Albany | $813 |
| Allegany | $706 |
| Bronx | $914 |
| Broome | $831 |
| Cattaraugus | $706 |
Monthly rates for a 40-year-old who's not eligible for subsidies.
Cheap New York health insurance plans by city
Ambetter from Fidelis Care has the cheapest health insurance in NYC, at an average rate of $675 per month for a Bronze plan.
Ambetter from Fidelis Care has the most affordable plans in all five of NYC’s boroughs. In fact, Ambetter from Fidelis Care has the cheapest rates for 98% of New York's population. There are only seven counties in New York where a company other than Ambetter from Fidelis Care has the cheapest rate.
Cheapest health insurance plans by NY county
County | Cheapest plan | Monthly rates |
|---|---|---|
| Albany | Ambetter from Fidelis Care Dep25 | $507 |
| Allegany | Ambetter from Fidelis Care Dep25 | $434 |
| Bronx | Ambetter from Fidelis Care Dep25 | $647 |
| Broome | Ambetter from Fidelis Care Dep25 | $509 |
| Cattaraugus | Ambetter from Fidelis Care Dep25 | $434 |
Cheapest Bronze plan with rates for a 40-year-old
Find Cheap Health Insurance Quotes in New York
What are Dep25 and Dep29 plans in New York?
In New York, dependents can stay on their parents' plan until age 29. Plans on NY State of Health are marked with "Dep25" or "Dep29" to indicate how long a dependent can stay on the plan. On Dep25 plans, you can only add a dependent up to age 25; with Dep29 plans, you can add a dependent between the ages of 25 and 29.
Dep29 plans cost more, and it's only worth paying for one if you have a dependent between age 25 and 29 to add to your plan.
Best health insurance by level of coverage
The best health insurance plan for you will depend on your medical needs, your financial situation and the plan availability in your area.
When deciding on the right plan, look for the plan tier that offers the right amount of coverage for your medical needs.
Platinum plans: Best for expensive medical treatment
| Platinum plans pay for about 90% of your medical care. |
Platinum plans cost $1,740 per month, on average, in New York.
Consider a Platinum health plan if you think you'll need a lot of expensive medical care in the coming year. For example, a Platinum plan may be a smart choice for someone who’s recently been diagnosed with cancer.
Platinum plans have expensive monthly rates, but you won't pay much when you visit the hospital. That's because Platinum plans typically have a low deductible and a low limit on how much you'll pay for medical care in a single year, called an out-of-pocket maximum.
Gold plans: Best if you have ongoing medical needs
| Gold plans pay for about 80% of your medical care. |
In New York, Gold plans cost $1,341 per month, on average.
A Gold plan is a good choice if you have to visit the hospital often. Gold plans come with expensive monthly rates, but you pay low costs when you get medical care.
Gold plans typically have low deductibles and cheap copays and coinsurance.
Silver plans: Best if you have a moderate income
| Silver plans pay for about 70% of your medical care. |
In New York, you'll pay an average of $1,090 per month for a Silver plan.
Silver plans have average monthly rates and middle-of-the-road costs when you go to the doctor. They’re usually a good choice for people with low incomes because they come with extra discounts.
In New York, you can also get a free plan called the Essential Plan if you make less than $39,125 per year. But if you make more than that, a Silver plan is a good choice.
Bronze plans: Best if you're generally healthy and can afford large medical bills
| Bronze plans pay for about 60% of your medical care. |
Bronze plans cost an average of $831 per month in New York.
A Bronze plan may be a good option if you're healthy and rarely visit the doctor. These plans have cheap monthly costs — however, you'll pay a high portion of the bill when you visit the doctor.
If you get seriously sick or injured with a Bronze plan, you could pay thousands of dollars before your coverage starts, which makes Bronze plans risky. You should only consider this coverage tier if you're healthy and have enough money in your savings account to cover a large, unexpected medical bill.
Bronze plans are popular in New York, making up half of all plans sold on NY State of Health. That's likely because of their cheap rates.
Catastrophic plans: Best as a last resort
You'll pay an average of $393 per month for a Catastrophic plan in New York.
Catastrophic plans have cheap monthly rates, but they don't pay for much of your health care. They're an option if you can't afford anything else. However, you should be aware that you'll have to pay up to $10,600 toward your health care bills in 2026 if you get sick or hurt.
You can only buy a Catastrophic plan if you're under 30 or otherwise qualify for an exemption. In addition, keep in mind that you cannot use premium tax credits to lower the monthly bill for a Catastrophic plan.
Free health insurance for New York residents who earn low incomes
New Yorkers have access to two types of free government health insurance: Medicaid and Essential health plans.
If you make too much for free health insurance, you may be eligible for extra discounts — called cost-sharing reductions (CSRs) — if you have a Silver health plan.
Medicaid: Best if you earn a low income
Medicaid provides free government medical insurance for New Yorkers who make about $22,000 per year or less as a single person or $44,000 per year or less for a family of four. The eligibility limits are higher for pregnant women and children.
Those who are age 65 and older may also qualify for cheap Medicare coverage.
Essential Plan: Free health insurance in New York
You can get free health insurance in NY through the Essential Plan if you make less than $39,125 per year as a single adult or under $80,375 per year as a family of four.
The Essential Plan is the best way to get affordable health insurance if you earn too much to qualify for Medicaid and don't have insurance through a job. You can sign up any time of the year, even if it's not open enrollment.
New York is just one of three states to offer this type of coverage to residents. These plans, called Basic Health Programs, help people who don't qualify for Medicaid but who would struggle to pay for regular health insurance.
However, funding for New York's Essential Plan is in danger. People making between $31,300 and $39,125 will no longer qualify for the Essential Plan starting in July 2026. An estimated 450,000 people could lose their coverage.
Use cost-sharing reductions for cheaper medical care
If you have a low income and a Silver plan, you might be able to get an extra discount that lowers the cost of your medical bills. These discounts are called cost-sharing reductions, and they lower the deductible, copay, coinsurance and out-of-pocket maximum on Silver plans.
To qualify, you have to make between $15,650 and $62,600 as a single person or $32,150 and $128,600 as a family of four. New York has a higher income limit for cost-sharing reductions than most states, which means more people can qualify and save on their medical bills.
If you qualify for cost-sharing reductions, check to see if you're eligible for an Essential Plan.
Are health insurance rates going up in NY in 2026?
On average, New York health insurance rates went up by 5% between 2025 and 2026.
Bronze and Platinum plans had the biggest increase, going up 10% and 9% each month, respectively, in 2026. Silver and Gold plans went up by 5% each month, while Catastrophic plans actually got 7% cheaper. Over the last five years, rates for most levels of health insurance in New York are up over 50%.
Catastrophic
Bronze
Silver
Gold
Platinum
Year | Cost | Change |
|---|---|---|
| 2025 | $423 | – |
| 2026 | $393 | -7% |
Monthly costs are for a 40-year-old.
Catastrophic
Year | Cost | Change |
|---|---|---|
| 2025 | $423 | – |
| 2026 | $393 | -7% |
Monthly costs are for a 40-year-old.
Bronze
Year | Cost | Change |
|---|---|---|
| 2022 | $525 | – |
| 2023 | $575 | 10% |
| 2024 | $646 | 12% |
| 2025 | $757 | 17% |
| 2026 | $831 | 10% |
Monthly costs are for a 40-year-old. Expanded Bronze plans are included in 2024, 2025 and 2026 averages, when they're offered.
Silver
Year | Cost | Change |
|---|---|---|
| 2022 | $713 | – |
| 2023 | $776 | 9% |
| 2024 | $873 | 13% |
| 2025 | $1,038 | 19% |
| 2026 | $1,090 | 5% |
Monthly costs are for a 40-year-old.
Gold
Year | Cost | Change |
|---|---|---|
| 2022 | $861 | – |
| 2023 | $940 | 9% |
| 2024 | $1,067 | 14% |
| 2025 | $1,272 | 19% |
| 2026 | $1,341 | 5% |
Monthly costs are for a 40-year-old.
Platinum
Year | Cost | Change |
|---|---|---|
| 2022 | $1,093 | – |
| 2023 | $1,181 | 8% |
| 2024 | $1,343 | 14% |
| 2025 | $1,590 | 18% |
| 2026 | $1,740 | 9% |
Monthly costs are for a 40-year-old.
Catastrophic plans only became available in New York in 2025.
Why is health insurance expensive in NY in 2026?
The cost of health care and prescription drugs is the biggest driver of rate hikes in 2026.
It's getting more and more expensive to go to the doctor, get lab work and tests and stay in the hospital. Because insurance pays for a large part of those costs for most people, rates have to rise so that the companies have enough money to pay for this medical care.
The cost and popularity of GLP-1 drugs, like Ozempic and Wegovy, is further impacting health insurance rates for 2026. When more people take an expensive medication, it means health insurance has to pay for more prescriptions. The company then increases rates to make sure it has enough money to cover the added costs.
Rates are also going up in 2026 because of changes to discounts, also known as subsidies. Since 2021, people with low incomes have been able to get higher subsidies. These were called "enhanced" subsidies, and they're expiring at the end of the year. Unless Congress acts to extend the enhanced subsidies, you can expect to pay more for health insurance even if you get discounts.
How to prepare for the 2026 rate increases
- Get quotes and shop around. Getting quotes and comparing health insurance plans from different companies can help you find the cheapest price for the coverage you need.
- Consider lowering your coverage. If you don't go to the doctor often, you might want to think about switching to a Bronze plan to save money. Plus, you can now get an HSA with Bronze plans, and that could help you save for the higher medical bills you'll have to pay. But a lower-tier plan isn't a good option for everyone, though — if you need to go to the doctor often or take prescription medications, a higher-tier plan is still probably the best option.
- Check if you can get discounts. If your income has recently dropped, see if you can get discounts. These can make the monthly rate of your health plan lower so it's easier to afford.
- Look into Medicaid or the Essential Plan. If you can't afford to buy insurance, check to see if you can get on Medicaid or if you qualify for New York's Essential Plan. These options give you free or cheap health insurance if you have a low income.
Obamacare in New York
You can apply for Obamacare plans in New York by going to NY State of Health, the state's health insurance exchange.
Obamacare or Affordable Care Act (ACA) plans offer special consumer protections. For example, plans can't charge you a higher rate or deny coverage based on your health. In addition, all plans have to cover specific services, also known as essential coverage.
Benefits that all NY Obamacare plans offer
- Outpatient care
- Emergency care
- Hospital care
- Care for pregnant women and newborns
- Preventive, wellness and ongoing disease services
- Prescription drugs
- Coverage for babies
- Laboratory services
- Rehabilitation services and devices
- Services for mental health and substance use disorders
Every ACA plan also has a limit on the amount you'll pay for medical care each year, called an out-of-pocket maximum.
Short-term health insurance in New York
New York bans short-term health insurance, as short-term plans don't have to offer essential benefits like maternity care, mental health care or prescription drugs.
New York state law requires all health insurance plans to offer these benefits.
Health insurance enrollment by income level in New York
The changes to health insurance subsidies in 2026 affect people with low incomes the most.
New York has a better safety net than many states, with Medicaid and the Essentials Plan available to people with low incomes. But more than 4 in 10 people with a plan from NY State of Health make less than about $60,000 per year. For people with already tight budgets, any change in rates or discounts can mean that health insurance becomes unaffordable.
Enrollment by income
Income | % of total enrollment |
|---|---|
| $37,651 to $45,180 | 17% |
| $45,181 to $60,240 | 24% |
| $60,241 to $75,300 | 10% |
| $75,301 or more | 11% |
| Other/Unknown | 37% |
Enrollment in 2025 marketplace plans made during the 2024-2025 Open Enrollment period. Total may not be 100% due to rounding
Frequently asked questions
What's the best cheap health insurance in New York?
MVP Health Care has the best health insurance in New York, with Bronze plans starting at $671 per month before discounts. But Ambetter from Fidelis Care sells cheaper Bronze plans, starting at $434 per month.
What is the most affordable health insurance in New York City?
Ambetter from Fidelis Care has the cheapest health insurance in NYC. Bronze plans start at $675 per month before discounts. But Anthem sells the best plans in NYC, starting at $822 per month for Bronze plans.
How can I get cheap health insurance in New York?
Health insurance tax credits (also known as subsidies) can reduce how much you pay for health insurance based on your income and family size. In New York, there’s also the Essential Plan, which provides free health insurance for people who have low incomes but don't qualify for Medicaid.
Is $200 a month expensive for health insurance in New York?
No, in New York, a $200 health insurance plan is very cheap. That's much cheaper than the state average of $831 per month for a Bronze plan. You could get health insurance for $200 per month if you qualify for discounted rates called subsidies.
Will ACA subsidies go away in 2026?
Subsidies likely won't go away entirely, but they might not save you as much money. For the last five years, the marketplace has had bigger discounts, called "enhanced subsidies" — those discounts expire at the end of 2025. Congress is currently debating how to move forward with subsidies, and laws could change quickly.
Methodology
New York health insurance rate data for 2026 is from NY State of Health, New York's state health insurance marketplace. ValuePenguin used the state marketplace data to find average rates for different plan tiers, geographic locations and family sizes.
Rates
Rates are based on a 40-year-old with a Bronze plan, unless otherwise noted. Rates for Bronze plans include regular and Expanded Bronze plans for 2024, 2025 and 2026, when the plans are available. Your costs and plan options will vary; plans aren't always available in all parts of a state or county.
Subsidies
Rates after subsidies are estimates for a 40-year-old with a Benchmark Silver plan and are based on how subsidies were structured before 2021. Prices are calculated using KFF's rates for full-price Benchmark plans, federal poverty levels (FPLs), IRS rules about premium tax credits and Congressional reports about expanded tax credits. The total cost in the state uses calculated rates by income, which are weighted using CMS data on the incomes of those who purchased plans during last year's open enrollment. The median was used for each income range. Unknown incomes were excluded from the calculations. Incomes of 100% of the federal poverty line and 500% of the federal poverty line were assumed for enrollees who earn less than 100% FPL and more than 500% FPL, respectively. Information about state subsidies, when available, was sourced from state marketplaces.
Ratings
ValuePenguin's experts rank companies based on cost, coverage options, customer satisfaction and unique value. Ratings are out of 100 possible points. ACA ratings show how the company performs in New York for medical care, member experience and plan administration. This 2026 plan quality data from CMS is based on data from last year. Ratings are not available for new plans or plans with low enrollment.
More sources
Enrollment trends, including plan selections by tier and enrollment by income, are from CMS data for the 2025 open enrollment period.
Info about causes of rate increases in 2026 is from the Peterson-KFF Health System Tracker. Other sources include KFF, the New York State Department of Health, S&P Global Capital IQ and the National Association of Insurance Commissioners (NAIC).
Insurance Writer
Cate Deventer is a ValuePenguin writer who specializes in health insurance, Medicare, auto and home insurance. She's been a licensed insurance agent since 2011.
She started her insurance career working as a customer service agent for State Farm. She later moved to an independent agency, where she worked with several insurance companies and hundreds of clients. She quoted policies, filed claims and answered insurance questions. In 2021, she pivoted her career and began writing about insurance for Bankrate. She moved to ValuePenguin in 2023 and began writing about health insurance and Medicare.
Cate has a passion for helping readers choose insurance to fit their needs. She enjoys knowing that her research and knowledge help people choose insurance products that make a positive difference in their lives.
How insurance helped Cate
Cate used her health insurance knowledge to navigate a surgery in 2023. Understanding how her policy worked let her focus on recovery instead of worrying about bills.
Expertise
- Health insurance
- Medicare & Medicaid
- Auto insurance
- Home insurance
- Life insurance
Credentials
- Licensed Life, Accident & Health Insurance Agent
- Licensed Property & Casualty Insurance Agent
Referenced by
- CBS
- NBC
- Wall Street Journal
Education
- BA, Theatre, Purdue University
- BA, English, Indiana University
Editorial note: The content of this article is based on the author's opinions and recommendations alone. It has not been previewed, commissioned or otherwise endorsed by any of our network partners.







