Best Cheap Health Insurance in Colorado for 2026
Kaiser Permanente is the best health insurance company in Colorado. Kaiser's cheapest Bronze plan costs $405 per month before discounts.
Find Cheap Health Insurance Quotes in Colorado
Best and cheapest health insurance in Colorado



Cheapest health insurance companies in Colorado
Select Health, Anthem, Elevate Health Plans and Kaiser Permanente have the cheapest health insurance plans in Colorado, with Bronze rates starting at $390 per month before discounts.

Find Cheap Health Insurance Quotes in Colorado
Affordable health insurance in Colorado
Company |
Cost
| |
|---|---|---|
| Select Health | $390-$513 | |
| Anthem | $394-$703 | |
| Elevate Health Plans | $403-$563 | |
| Kaiser Permanente | $405-$486 | |
- Select Health has the cheapest Bronze plans for 4 out of 5 people in Colorado, with coverage starting at $390 per month.
- Kaiser Permanente offers the most affordable Silver health insurance in Colorado, with plans that cost as little as $500 per month. Kaiser has the cheapest Silver coverage for 9 out of 10 Coloradans.
- Elevate Health Plans has the cheapest Gold medical insurance in Colorado, with rates as low as $480 per month. The company has the best Gold quotes for 2 out of 5 people in Colorado, including those in Denver and Aurora. Kaiser Permanente has the cheapest Gold coverage for about one-third of Coloradans, including people who live in Colorado Springs and Fort Collins.
Both Anthem and Rocky Mountain Health Plans are going to be harder to get in Colorado in 2026. The plans won't be available in much of the Front Range area, especially around Denver.
Anthem plans to stop selling its health insurance in 16 counties. Rocky Mountain Health Plan intends to stop selling plans in seven counties. This means that around 96,000 individuals could have to shop for a new health plan in 2026.
However, Anthem has noted that it could still change course and continue selling plans in some or all of these counties.
Best health insurance companies in Colorado
Kaiser Permanente is the best health insurance company in Colorado, earning a perfect 5-star rating from Connect for Health Colorado.
Kaiser Permanente is known for its excellent customer service and high-quality medical care, which is why it's the only 5-star rated company in Colorado. It's also the most popular health insurance company in Colorado, selling about half the health insurance plans in the state.
The downside of Kaiser Permanente is that you can usually only see the doctors at Kaiser's medical facilities.
Find Cheap Health Insurance Quotes in Colorado
Best-rated health insurance companies in CO
Company |
ACA rating
|
VP rating
|
|---|---|---|
| Kaiser Permanente | ||
| Rocky Mountains Health Plans | ||
| Select Health | N/A | |
| Cigna | ||
| Anthem |
How much does individual health insurance cost in Colorado?
Health insurance in Colorado costs an average of $703 per month if you pay full price for a Silver health plan or an estimated $251 per month if you qualify for discounts based on your income.
Find Cheap Health Insurance Quotes in Colorado
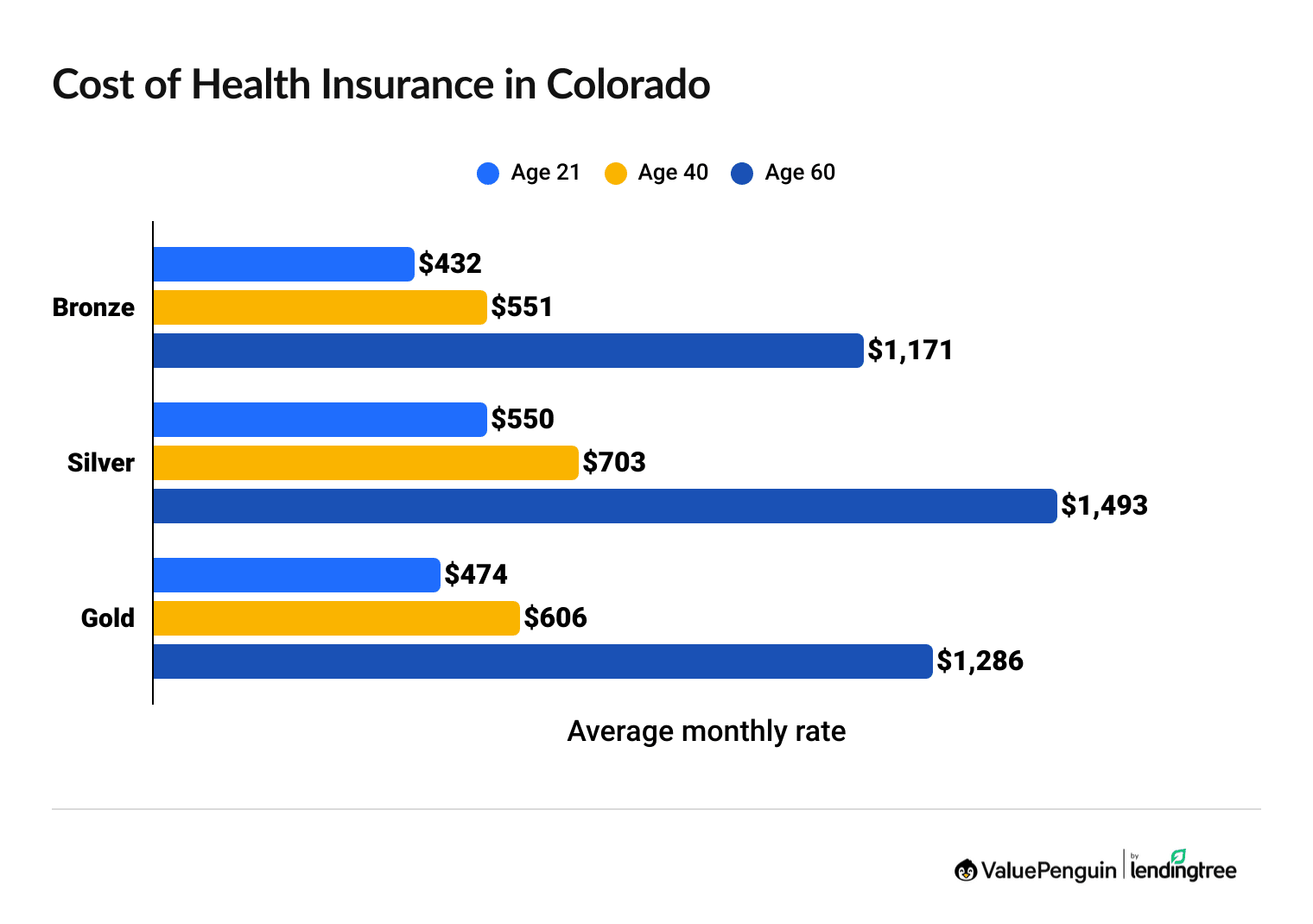
Your health insurance rates are based on your age, the plan you choose and your income.
- Younger people typically pay less each month.
- Lower plan tiers like Bronze are usually cheaper but offer less coverage.
- If you qualify for subsidies, rates are on a sliding scale based on your income.
In Colorado, it usually costs more to buy a Silver plan than a Gold plan, even though the Gold plans have better coverage. If you're looking at a Silver plan, compare your options for Gold, too. You might find that you can get more coverage at a lower price. However, a Silver plan will be the best deal if you can get extra discounts on your medical costs because of your income, which are only available with Silver health plans.
Health insurance discount changes in Colorado for 2026
A Silver health insurance plan costs $703 in Colorado or roughly $251 per month, on average, if you're eligible for discounts because of your income.
The cost of a Silver health insurance plan will rise from about $197 in 2025 to $251 in 2026 after discounts, called subsidies. That's because discount levels are getting smaller for 2026.
Between 2021 and 2025, you could get larger discounts, called "expanded subsidies." These larger discounts won't be available in 2026. While you can still get discounts depending on your income, they'll be smaller than in years past.
Health insurance rates in Colorado after subsidies (2025 vs. 2026)
Income | 2025 rate | 2026 rate | Difference |
|---|---|---|---|
| $30,000 | $49 | $75 | 53% |
| $40,000 | $154 | $207 | 34% |
| $50,000 | $283 | $335 | 18% |
| $60,000 | $423 | $418 | -1% |
| $70,000+ | $463 | $557 | 20% |
Average cost after subsidies for a single 40-year-old with a Benchmark Silver plan.
- Who can get subsidies? To get subsidies, you need to earn between $15,650 and $62,600 as an individual ($32,150 to $128,600 for a family of four). The less you make, the larger your discount.
- How do subsidies work? You can use your subsidy on any Bronze, Silver or Gold plan bought through Connect for Health Colorado. The government will let you choose to either automatically apply your discount to your monthly rate or get your entire subsidy as a lump sum when you file your taxes. You don't have to take any special steps to get a subsidy. The government will automatically calculate and apply what it believes you'd get based on your income.
- How much do you save? Use ValuePenguin's subsidy calculator to find out how much you'll pay for coverage after subsidies.
Cheap Colorado health insurance plans by city
Select Health has the cheapest health insurance in the Denver metro area, Colorado Springs and Fort Collins.
Select Health has the most affordable coverage nearly everywhere in Colorado, including the state's 10 largest cities.
County | Cheapest plan | Monthly rates |
|---|---|---|
| Adams | Select Health Value Bronze | $402 |
| Alamosa | Anthem Colorado Option Bronze Pathway | $515 |
| Arapahoe | Select Health Value Bronze | $402 |
| Archuleta | Anthem Colorado Option Bronze Mountain Enhanced | $511 |
| Baca | Anthem Colorado Option Bronze Pathway | $515 |
Cheapest Bronze plan with rates for a 40-year-old
Find Cheap Health Insurance Quotes in Colorado
Best health insurance by level of coverage
In Colorado, the best health insurance plan for you depends on your monthly budget and how much medical care you need.
Gold plans: Best if you need frequent medical care
| Gold plans pay for about 80% of your medical care. |
Gold plans cost an average of $606 per month in Colorado.
Gold plans have the best coverage. If you need ongoing or complex medical care, Gold plans can save you money overall. They'll help you save on medical costs because of their low deductibles, coinsurance and copays.
Silver plans: Best if you have a low income to get discounts
| Silver plans will pay 73% to 94% of your medical costs if you have a low income. |
In Colorado, Silver plans cost an average of $703 per month. This means that Silver plans are often more expensive than Gold in the state. So if you don't qualify for medical cost reductions, check if a Gold plan is more affordable than Silver where you live.
If you earn less than about $39,000 per year as an individual or $80,000 per year as a family of four, you'll usually get the best deal with a Silver plan because of a program where you can get discounts on your medical bills.
The cost-sharing reduction program improves your medical coverage if you qualify. But the program is only available if you choose a Silver plan.
Bronze plans: Best if you're young and healthy
| Bronze plans pay for about 60% of your medical care. |
Bronze plans have the cheapest monthly rates, with an average rate of $551 per month. They can be good if you are healthy and don't need much medical care. But you'll have to pay a larger part of your medical bills.
A Bronze plan will help you save overall if you only go to the doctor a few times per year. You also don't need to meet your deductible before coverage starts for preventive care, and your medical bills will be capped if you get very sick or badly injured.
However, your costs for expensive treatment can be high before the plan's full benefits kick in. Be sure you have enough savings to pay for a medical emergency if you choose a Bronze plan.
Medicaid: Free health insurance if you have a low income
If you make less than about $22,000 as a single person or roughly $44,000 as a family of four, Medicaid is the best health insurance option. You'll get great coverage for free or very little cost.
Medicaid is a federal program for people with low incomes. Even if you have a higher household income, you might still qualify for Medicaid if you are pregnant or under age 19.
You can apply for Medicaid in Colorado through Health First Colorado, where you can also check your benefits or find a doctor after you're enrolled.
Are health insurance rates going up in Colorado?
The average cost of health insurance in Colorado increased by about 24%, on average, between 2025 and 2026.
Silver and Bronze plan rates increased the most, by an average of 27% and 24% respectively. Gold plan prices rose by only 20%, on average. The average cost of a Silver health plan in Colorado rose by 72% between 2022 and 2026.
Bronze
Silver
Gold
Year | Cost | Change |
|---|---|---|
| 2022 | $413 | – |
| 2023 | $354 | -14% |
| 2024 | $386 | 9% |
| 2025 | $445 | 15% |
| 2026 | $551 | 24% |
Monthly costs are for a 40-year-old. Expanded Bronze plans are included in 2024, 2025 and 2026 averages, when they're offered.
Bronze
Year | Cost | Change |
|---|---|---|
| 2022 | $413 | – |
| 2023 | $354 | -14% |
| 2024 | $386 | 9% |
| 2025 | $445 | 15% |
| 2026 | $551 | 24% |
Monthly costs are for a 40-year-old. Expanded Bronze plans are included in 2024, 2025 and 2026 averages, when they're offered.
Silver
Year | Cost | Change |
|---|---|---|
| 2022 | $409 | – |
| 2023 | $489 | 20% |
| 2024 | $535 | 9% |
| 2025 | $554 | 4% |
| 2026 | $703 | 27% |
Monthly costs are for a 40-year-old.
Gold
Year | Cost | Change |
|---|---|---|
| 2022 | $420 | – |
| 2023 | $465 | 11% |
| 2024 | $459 | -1% |
| 2025 | $505 | 10% |
| 2026 | $606 | 20% |
Monthly costs are for a 40-year-old.
Why is health insurance expensive in CO in 2026?
The rising cost of health care is causing health insurance rates to go up in 2026.
When health care gets more expensive, health insurance companies spend more money when people go to the doctor. To make up for that, companies charge higher rates for everyone. The high cost and popularity of GLP-1 drugs like Ozempic and Wegovy is also causing rate increases.
Another cause of high rates in 2026 is changes to marketplace discounts, called subsidies. Since 2021, people with low incomes have gotten bigger discounts, called "enhanced subsidies." These larger discounts will expire at the end of 2025. This means that you'll pay more for health insurance even if you can still get a discount.
How to prepare for the 2026 rate increases
- Shop around. If your plan goes up, check to see if there are cheaper plans in your area. Different companies have different rates, and you might find a plan that works for you but costs less each month.
- Lower your coverage. If you need a cheaper plan, you could consider a lower tier, like Bronze. Just remember that you have to pay for more of your health care with a Bronze plan. However, you can now open an HSA with Bronze plans, and that can help you save for medical costs.
- Check for discounts. Even though discounts may not be as good in 2026, you should still see if you qualify. Subsidies are based on your income, and the less you make, the more you'll save.
- See if you can get Medicaid. If you make less than about $22,000 per year as a single person or less than $44,000 per year as a family of four, you can probably get on Colorado Medicaid. This is usually free or very inexpensive and pays for most of your medical care.
Colorado insurance marketplace: Connect for Health
All marketplace health insurance plans have important benefits to protect your health and finances.
- You get free checkups and preventive care as soon as the plan begins.
- You won't be denied coverage or pay more for a plan if you have a preexisting condition.
- All plans protect you from major medical debt through the out-of-pocket maximum.
Short-term health insurance in Colorado
You can't buy short-term health insurance in Colorado. The state changed its rules for short-term health insurance in 2019. Although short-term health insurance is allowed in Colorado, no insurance companies sell short-term policies.
Health insurance enrollment by income level in Colorado
More than half of all people in Colorado with marketplace coverage earn less than $45,180 per year.
People who make low incomes tend to use Connect for Health Colorado to get coverage more often than other groups. That means lower subsidies in 2026 will disproportionately affect those who earn less money.
Enrollment by income
Income | % of total enrollment |
|---|---|
| Less than $15,060 | 1% |
| $15,060 to $20,783 | 2% |
| $20,784 to $22,590 | 7% |
| $22,591 to $30,120 | 18% |
| $30,121 to $37,650 | 11% |
Enrollment in 2025 marketplace plans made during the 2024-2025 Open Enrollment period. Total may not be 100% due to rounding
Frequently asked questions
What is the cheapest health insurance in Colorado?
Select Health has the cheapest Bronze plan in Colorado, at $390 per month. That's about 29% cheaper than the CO state average. Select Health has the most affordable coverage for more than 4 out of every 5 people in Colorado, including people in Denver, Colorado Springs and Fort Collins.
What is the best health insurance company in Colorado?
Kaiser Permanente is the best health insurance company in Colorado. It has a perfect five-star rating from Connect for Health Colorado and consistently high customer satisfaction reviews. Kaiser Permanente also has the cheapest Silver plans in Colorado, with coverage starting at $500 per month. And Kaiser Permanente is the most popular health insurance company in Colorado, selling more than half of all health insurance plans in the state.
Is $500 a month normal for health insurance?
$500 per month is actually cheaper than average for health insurance in Colorado. On average, Bronze plans cost $551 per month, Silver plans cost $703 per month and Gold plans cost $606 per month. You might get a cheaper rate if you have a low income and can get discounts.
How much does Obamacare cost in Colorado?
A Bronze Obamacare policy from Colorado's state marketplace costs an average of $551 per month. However, the estimated cost of an Obamacare plan after discounts, called subsidies, is $251 per month, on average.
Is Select Health Insurance good in Colorado?
Select Health has the cheapest Bronze plans for most people in Colorado, with rates starting at $390 per month. Select Health doesn't yet have a rating from the Colorado state marketplace. That doesn't mean it's a bad company, but some people might prefer choosing a company with an established track record.
How do I get health insurance in Colorado?
Most people in Colorado get health insurance from their jobs. If you need to buy a plan yourself, you can shop on Connect for Health Colorado, the state's health insurance marketplace. You can also buy a plan directly from an insurance company, but you won't be able to get discounts that way.
Methodology
Colorado health insurance rate data for 2026 is from Connect for Health Colorado. ValuePenguin used the Connect for Health Colorado marketplace to find average rates for different plan tiers, geographic locations and family sizes.
Rates
Rates are based on a 40-year-old with a Silver plan, unless otherwise noted. Rates for Bronze plans include regular and Expanded Bronze plans for 2024, 2025 and 2026, when the plans are available. Your costs and plan options will vary; plans aren't always available in all parts of a state or county.
Subsidies
Rates after subsidies are estimates for a 40-year-old with a Benchmark Silver plan and are based on how subsidies were structured before 2021. Prices are calculated using KFF's rates for full-price Benchmark plans, federal poverty levels (FPLs), IRS rules about premium tax credits and Congressional reports about expanded tax credits. The total cost in the state uses rates calculated by income, which are weighted using CMS data on the incomes of those who purchased plans during last year's open enrollment. The median was used for each income range. Unknown incomes were excluded from the calculations. Incomes of 100% of the federal poverty line and 500% of the federal poverty line were assumed for enrollees who earn less than 100% FPL and more than 500% FPL, respectively. Information about state subsidies, when available, was sourced from state marketplaces.
Ratings
ValuePenguin's experts rank companies based on cost, coverage options, customer satisfaction and unique value. Ratings are out of 100 possible points. ACA ratings show how the company performs in Colorado for medical care, member experience and plan administration. This 2026 plan quality data from CMS is based on data from last year. Ratings are not available for new plans or plans with low enrollment.
More sources
Enrollment trends, including plan selections by tier and enrollment by income, are from CMS data for the 2025 open enrollment period.
Other sources include S&P Global Capital IQ and the National Association of Insurance Commissioners (NAIC).
Senior Writer
Talon Abernathy is a ValuePenguin Senior Writer who specializes in health insurance, Medicare and Medicaid. He's also contributed to other insurance verticals including home, renters, auto, motorcycle and flood insurance.
Talon came to ValuePenguin in 2023. Since his arrival, he's helped to expand the site's health insurance-related content offerings. He enjoys helping readers understand the ins and outs of America's all too complicated health insurance landscape.
Before coming to ValuePenguin, Talon worked as a freelance writer. His prior work has touched on a broad range of personal finance-related topics including credit-building strategies, small business incorporation tactics and creative ways to save for retirement.
Insurance tip
In many parts of the country, you can qualify for a free Silver health insurance plan if you meet certain income requirements. Government subsidies in the form of premium tax credits and cost-sharing reductions may mean you'll pay nothing for coverage.
Expertise
- Health insurance
- Medicare and Medicaid
- Flood insurance
- Homeowners insurance
- Renters insurance
- Auto and motorcycle insurance
Referenced by
- The Miami Herald
- Money.com
- MSN
- Nasdaq
- The Sacramento Bee
- Yahoo! Finance
Education
- BA, University of Washington
- Certificate in Copyediting, UC San Diego
Credentials
- Licensed Life & Disability Insurance Agent
- Licensed Property & Casualty Insurance Agent
Editorial note: The content of this article is based on the author's opinions and recommendations alone. It has not been previewed, commissioned or otherwise endorsed by any of our network partners.




