Long-Term Care Insurance: Is it Worth the Cost?
Find Cheap Life Insurance Quotes in Your Area
Long-term care (LTC) insurance provides financial assistance for people living with chronic illnesses and disabilities. This is usually seniors who need help performing essential tasks such as eating, bathing, dressing and taking care of their homes. In most instances, long-term care insurance provides coverage for nursing home care, home health care and personal or adult day care.
How much does a long-term care insurance plan cost?
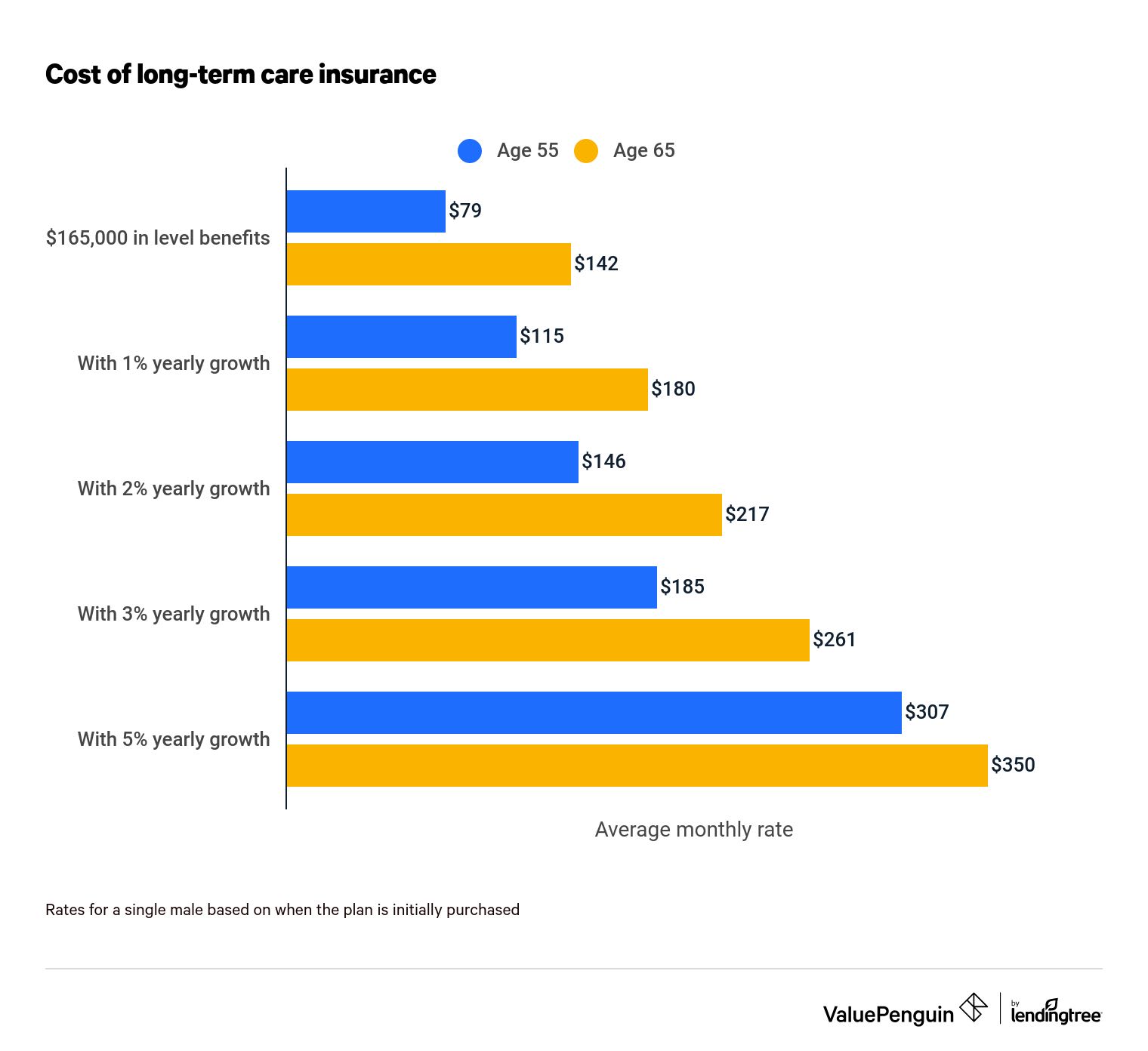
A 55-year-old male will pay about $79 per month for a long-term care insurance plan with $165,000 in benefits.
However, the costs of long-term care insurance vary widely, and rates can be as high as $600 per month depending on your situation, how much the policy is worth and how much coverage it provides.
The following factors all play a role in determining the cost of a policy:
- Maximum daily benefits paid out
- The extent of covered services
- Your age and health status when purchasing the policy
- The elimination period
- Your gender
A policy's benefits can grow over time
With most policies, beneficiaries have the option of purchasing coverage with level benefits — meaning they stay the same during the course of the policy — or benefits with built-in growth rates that grow annually as a way to keep pace with inflation.
Policies with built-in growth rates cost more than policies with level benefits. For example, a 55-year-old male would pay about twice as much for a plan that has benefits that increase 3% annually.
What’s the cost of long-term care insurance by age?
If you're age 55, the monthly cost of a long-term care insurance policy will typically increase 24% if you delay enrolling until age 60, and will increase an additional 45% between age 60 and 65.
Long-term care insurance costs
Policy benefits | Age 55 | Age 60 | Age 65 | Increase (age 55 vs. 65) |
|---|---|---|---|---|
| $165,000 in level benefits | $79 | $98 | $142 | 79% |
| With 1% yearly growth | $115 | $133 | $180 | 57% |
| With 2% yearly growth | $146 | $167 | $217 | 49% |
| With 3% yearly growth | $185 | $294 | $261 | 41% |
| With 5% yearly growth | $307 | $317 | $350 | 14% |
Rates for a single male based on when the plan is initially purchased
The age at which you enroll plays a significant role in determining policy costs. A single man purchasing a plan with $165,000 in level benefits could expect to pay $79 per month at age 55. If that man purchases the same policy at age 60, he will pay about $98 per month in premiums. That same policy climbs to $142 in monthly premiums if the man waits until the age of 65 to buy the policy.
For couples, purchasing a joint policy is a good way to save money on premiums.
A couple, both of whom are 55, can expect to pay about $173 per month for a policy providing $165,000 in level benefits. That would be about a $31 monthly savings as compared to individually purchasing a policy for a male and a female.
What is long-term care insurance?
Long-term care insurance helps pay for medical and nonmedical care when you’re unable to perform daily activities on your own.
Long-term care services are expensive and are not covered by Medicare or regular health insurance. This could mean you'd pay the full cost of these services unless you have additional coverage. A long-term care insurance policy is a way to protect your assets against the possibility that you may need these services as you age.
A long-term care policy helps with the cost of care provided in the following venues:
- Your home
- Nursing homes
- Adult day service centers
- Assisted living facilities
- Alzheimer’s special care facilities
Some policies help pay for in-home care services, including housekeeping, cooking and cleaning support.
In a typical case, you’d purchase a long-term care policy while you're still healthy, choosing a set of benefits you think you’ll need and paying on the policy every month as you age. You could pay monthly premiums for years or, in some cases, decades before actually needing long-term care services and coverage.
When will a long-term care insurance plan provide benefits?
With most long-term care policies, you qualify for benefits after a health care provider certifies you can no longer perform two of the following Activities of Daily Living (ADLs) without direct hands-on assistance. ADLs include:
- Bathing
- Eating
- Walking
- Dressing
- Transferring (going from a bed to a chair)
- Going to the bathroom
Beneficiaries may also qualify for long-term care benefits as a result of a severe cognitive impairment such as Alzheimer’s disease or dementia.
When should you sign up for a long-term care insurance policy?
The best time to purchase a long-term care insurance policy is in your 50s, when you are still in relatively good health.
The two most important factors to consider are your age and your medical condition.
Age
Medical condition
How old you are will affect how much you pay for a plan. As a general rule, the older you are, the more expensive your policy is. If you wait too long to purchase a plan, the high cost of coverage may make a plan unaffordable. And if you wait past a certain age to try to purchase a policy — usually your mid-70s — you are probably going to be denied coverage by the insurance company.
Age
How old you are will affect how much you pay for a plan. As a general rule, the older you are, the more expensive your policy is. If you wait too long to purchase a plan, the high cost of coverage may make a plan unaffordable. And if you wait past a certain age to try to purchase a policy — usually your mid-70s — you are probably going to be denied coverage by the insurance company.
Medical condition
Additionally, you have to qualify based on your health status when applying for a long-term care insurance policy. This means you are going to have to answer a battery of questions about your health. You are probably going to have to take a physical examination as well.
Long-term care policies are typically only issued to relatively healthy people because they represent a high risk for insurance companies. It should be stressed that qualifying for a policy is not automatic. There are currently only six companies in the United States selling standalone long-term care policies, and these companies routinely reject applicants based on health status or preexisting conditions.
Is a long-term care insurance policy worth it?
A long-term care insurance policy is usually worth it for most people because it protects against the risk of paying for nursing home, assisted living or custodial care.
Without coverage, your out-of-pocket expenses for long-term care could be more than $54,000 per year.
Long-term care service | Annual cost | |
|---|---|---|
| Assisted living facility | $64,200_ In-home care homemaker services | $68,640 |
| In-home care health aide | $75,504 | |
| Private room nursing home | $116,800 |
National median costs
- 70% of people 65 and older will need long-term care
- 48% of people older than 65 will receive paid long-term care at some point in their lives
The costs of long-term care services are staggering, easily outstripping many household budgets and depleting retirement savings in some cases. Because of this, long-term care insurance can mean the difference between solvency and bankruptcy, ultimately determining whether you are able to access life-sustaining and lifesaving care in many cases.
While it's common for family members to provide unpaid care, the extent of care will vary from a few months to several years.
When is a long-term care insurance policy not worth it?
While long-term care insurance has its uses and purposes, it is not for everyone. A plan may not be worth it in the following situations:
- If your payments exceed 7% of your monthly expenses
- If you're in your 30s or 40s
- If you have significant financial resources
- If you're willing to leverage other assets
Even when you buy a plan, there is always the chance you will never need to use your coverage, making long-term care insurance a true use-it-or-lose-it proposition. If you don’t use it, you don’t get benefits from it, aside from knowing that you are insured against the risk of needing expensive long-term care.
Example: Larry, a single 60-year-old earning more than $150,000 a year, wants financial protection in case he needs long-term care. He takes out a long-term care insurance policy:
- Policy: $165,000 in benefits with a growth rate of 2% a year
- Cost: $275 per month ($66,000 over 20 years)
Uses insurance
Does not use insurance
In this potential scenario, when Larry turns 80, he develops Alzheimer’s disease and moves to a nursing home that costs $100,000 a year. Larry spends two years in the nursing home, running up $200,000 in bills before dying of Alzheimer’s at the age of 82. But fortunately, Larry has a long-term care insurance policy with benefits that have been growing at 2% a year. This provides him with $231,000 in covered benefits, more than enough to meet his nursing home bills.
Uses insurance
In this potential scenario, when Larry turns 80, he develops Alzheimer’s disease and moves to a nursing home that costs $100,000 a year. Larry spends two years in the nursing home, running up $200,000 in bills before dying of Alzheimer’s at the age of 82. But fortunately, Larry has a long-term care insurance policy with benefits that have been growing at 2% a year. This provides him with $231,000 in covered benefits, more than enough to meet his nursing home bills.
Does not use insurance
In another scenario, Larry buys the same policy at age 60, paying on the policy well into his 80s. But in this situation, Larry does not develop Alzheimer’s disease and lives until the age of 85 before dying of natural causes. He pours more than $82,500 into a policy he never uses.
How are long-term care insurance benefits paid?
Most long-term care policies pay out on a daily basis, paying the facility or provider a daily amount to cover the costs of your care.
Please note that the federal government will tax long-term care insurance benefit amounts that exceed $390 a day in 2022. So, for example, if your policy pays out $500 a day, you will have to pay taxes on the $110 over the $390 daily limit.
This is known as a reimbursement policy, and daily amounts range anywhere from $50 to more than $500 depending on the policy.
Some policies pay out through a cash indemnity, sending you a check or depositing money into your account, usually on a monthly basis so you can then pay the health care facility or health care provider. If the monthly amount exceeds $390 a day, then the federal government will tax the amount over the $390 nontaxable limit.
Find Cheap Life Insurance Quotes in Your Area
Understanding your options when choosing a plan
Level benefits vs. growth
One of the first things to look for in a policy is protection against inflation. And that means buying a policy with a built-in growth rate to mitigate the effects of rising prices. That added protection costs money, doubling or, in some cases, tripling the cost of certain policies.
Your costs
There are other considerations when purchasing a policy — how much insurance you are interested in purchasing, for example, and how much you are willing to spend on a policy.
Exclusionary period
Most policies impose a 90-day waiting period between the time you qualify for a policy and when coverage actually begins, forcing you to pay for the coverage during that exclusionary period.
Preexisting conditions
You may also be offered a long-term care insurance policy with an exclusion for preexisting conditions. This could be a temporary exclusion, not covering the costs of the preexisting condition for a certain amount of time, usually six months. Or it could be broader, and for example, an insurance company could not pay any costs associated with a preexisting condition such as heart disease.
As a general rule, long-term care policies will not cover costs resulting from alcoholism or drug addiction.
Shared care
With some plans, couples can purchase a shared care policy, which costs more but allows one spouse to tap into the plan benefits of the other spouse, if needed.
Let’s say, for example, that a husband and wife take out separate long-term care policies worth $500,000 each. The husband develops Alzheimer’s disease and spends three years in a nursing home that costs $150,000 a year, depleting the husband's long-term care benefits.
The wife remains relatively healthy and does not use her benefits, leaving her $500,000 worth of long-term care benefits intact. Under a shared care policy, the husband can become a "rider" on the wife’s plan, tapping into her benefits to pay for the nursing home.
Hybrid insurance policies
Not surprisingly, many beneficiaries do not like the use-or-lose-it premise of long-term care insurance. As a result, some beneficiaries turn to hybrid insurance policies linking their life insurance policies with a long-term care policy that can be used to pay for long-term care expenses as well as a death benefit when the insured beneficiary dies.
With these life insurance policies with a long-term care rider, the insured is able to leave some money for their beneficiaries at the time of death, recouping some of the costs of the policy even if the insured does not use the long-term care benefit. These types of policies tend to be more expensive than traditional policies.
Long-term care insurance vs. other types of insurance
People often confuse long-term care insurance with regular health insurance and disability insurance even though these types of insurance policies are vastly different.
Health insurance
Regular health insurance covers medical care, helping to pay for medical bills resulting from sickness and injuries as well as physician and hospital visits. It does not pay for long-term care in most instances.
In contrast, long-term care insurance is more about maintenance, assisting beneficiaries with the support costs for daily activities.
Long-term disability insurance
Long-term disability insurance pays for lost income, replacing a portion of income forfeited because you are unable to work as a result of an injury or sickness.
Medicare
Medicare does not provide a benefit for long-term custodial care or care for chronic conditions. Medicare, available to seniors and those who have disabilities, provides limited benefits for nursing home stays, paying only for acute, temporary conditions immediately following hospitalization. If your disability is chronic rather than acute, long-term services are not covered under Medicare.
Medicaid
Medicaid does provide assistance for long-term care needs, but only for those who meet strict income and asset limits. Eligibility for Medicaid varies by state, and for example, an individual would need to earn less than $21,597 per year in a state with expanded Medicaid.
In order to qualify for Medicaid's long-term care benefits, you may need to liquidate your assets to meet your state's requirements. You may also need to pay for a portion of your long-term care out of pocket and use the Medicaid spend down program, which is designed for "medically needy" individuals as a way to use medical expenses to help you qualify.
There are sometimes risks to using Medicaid to pay for long-term care. Depending on your state, if Medicaid pays long-term care benefits, officials may be able to seize your assets after your death or the death of your spouse if your spouse survives you.
Frequently asked questions
How much does long-term care insurance cost?
A 55-year old male pays an average of $79 per month for a $165,000 long-term care policy with level benefits, and the same policy costs an average of $142 per month if purchased at age 65. However, costs vary depending on the policy and how much it covers.
What’s the biggest drawback of long-term care insurance?
The biggest drawback of traditional long-term care insurance is that you could pour thousands and thousands of dollars into a policy and never use it, leaving you without any tangible financial benefits. Another major drawback is that your initial policy application could be denied based on your health status.
What’s the best age to buy a long-term care insurance plan?
The best time to buy a plan is between your mid-50s and your early-60s when you are still relatively healthy and can qualify for a policy. Purchasing a policy within this time frame will help ensure that you don’t pay too much for a policy, which is likely to happen if you purchase a policy in your 30s or even 40s and don’t need coverage until you are in your 80s.
Sources
Insurance Writer
Jim Arvantes, a former freelance writer for ValuePenguin, has worked in the health care field for more than 20 years, reporting and writing for a variety of publications and covering many issues, including HIV/AIDS, infectious diseases in prisons and jails, and ongoing efforts to reform the nation’s health care system. For nearly seven years, Jim served as the Washington Correspondent for AAFP News, the online news source for the American Academy of Physicians. In that role, Jim wrote both news and feature articles that focused on the role of primary care in improving health care, enhancing health care access and reducing health care costs.
He has developed an expertise in many areas of the health care field, including the Affordable Care Act, payment and delivery reform as well as the Medicaid and Medicare programs. Jim relied on his expertise and vast experiences as a former health care writer when he covered stories for ValuePenguin.
Editorial Note: The content of this article is based on the author's opinions and recommendations alone. It has not been previewed, commissioned or otherwise endorsed by any of our network partners.